Check out the summary on AHA/ACC hypertension guidelines chat, done by NephJC intern Sridatta Pawar
ASIs Advance: NephJC Shorts on BaxHTN
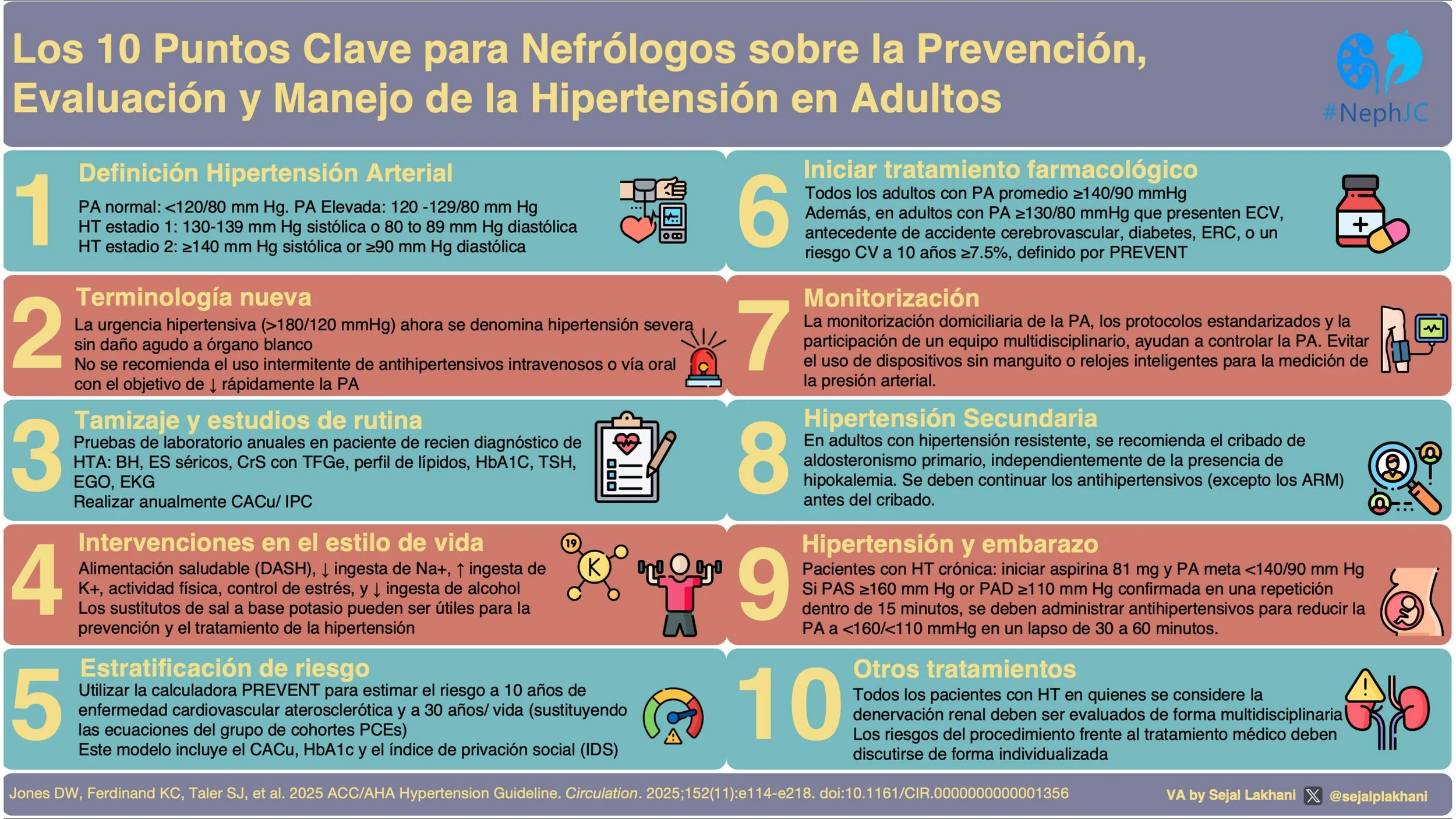
Guías AHA/ACC 2025 en Hipertensión: el resumen visual
La hipertensión arterial sigue siendo uno de los principales factores de riesgo modificables para enfermedad cardiovascular y enfermedad renal crónica. Las nuevas guías AHA/ACC 2025 han actualizado aspectos fundamentales sobre la prevención, la evaluación y el tratamiento de la hipertensión, con implicaciones directas para la práctica nefrológica.
Revisa el resumen visual creado por Dr Sejal Lakhani
visual abstract, Visual Abstract, sejal lakhani, Hypertension, HTN, ACC/AHA, 2025
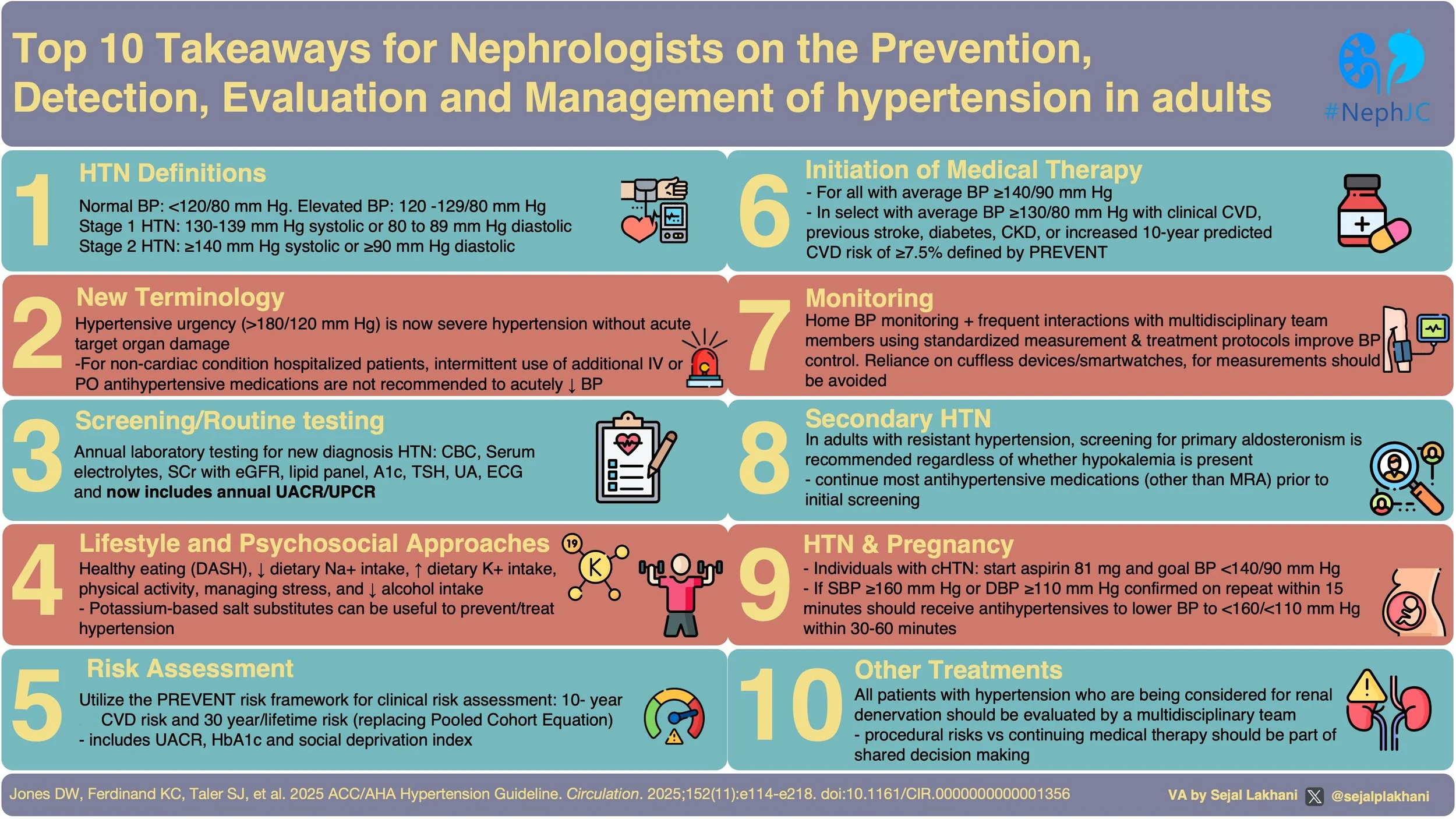
The AHA/ACC 2025 Hypertension Guidelines visual abstract
New updated guidance on hypertension including screening for secondary causes, use of renal denervation, hypertension and pregnancy, risk assessment, monitoring and treatment.
Check out this wonderful VA by Dr Sejal Lakhani
PREVENT, Detect, Treat: What’s New in the 2025 Hypertension Toolkit
Advance-HTN: Return of the systolic order – Lorundrostat’s role in restoring balance
Does Lorundrostat Effectively Lower Blood Pressure in Uncontrolled Hypertension?
Stunning visual abstract summarizing NEJM study, by Priti Meena
Is a lower BP the road to better outcomes in diabetes?
How low is too low for blood pressure? Will BPROAD get to the bottom of this issue?
Underestimating primary aldosteronism?
Should we screen all individuals with hypertension for primary aldosteronism?
Hunting Primary Hyperaldosteronism: are MRAs a blindfold in adrenal vein sampling?
Undercover Aldosterone
BPROAD: Sprinting down the BP Road in Diabetes
The pressure is on! Unravelling the ESPRIT of Intensive vs Standard BP Control
This week, we will discuss the ongoing saga of blood pressure targets in patients with hypertension. This time its ESPRIT (Effects of Intensive Systolic Blood Pressure Lowering Treatment in Reducing Risk of Vascular Events) making a case for case for intensive BP control in most hypertensive individuals, including those with a history of diabetes and stroke.
NephJC Rewind: PATH-BP
We have been doing NephJC for over ten years and we feel, in that time we have covered the most important manuscripts in nephrology. With a decade of history NephJC has covered a large amount of the clinical evidence used in day to day clinical care. In fact I find myself sending links to old NephJC summaries pretty commonly and we would like to surface some of these older summaries from time to time. So here is out first NephJC Rewind
Last week JAMA Internal Medicine published this manuscript any Tim Anderson, Management of Elevated Blood Pressure in the Hospital—Rethinking Current Practice. Here, Dr. Anderson is trying to operationalize the work he has been doing for quite some time demonstrating the lack of efficacy and frank harm caused by treating inpatient hypertension. This has been explored in NephJC, Freely Filtered, and NephMadness. As part of this manuscript he supplied a flow chart that showed acetaminophen as a cause of hypertension:
I tweeted about this and a number of people asked about acetaminophen being listed as a cause of drug induced hypertension. This is where PATH-BP comes in (MacIntyre, Circulation 2022). This was a well done cross over trial with a two week washout. Patients took a gram of acetaminophen four times a day or a matched placebo.
The primary outcome was a change in mean daytime systolic ambulatory BP.
There was a statistically significant increase in mean daytime systolic ambulatory BP of 4.7 mm Hg (95% CI, 2.9-6.6; P<0.0001) with acetaminophen compared with placebo.
This was not a mechanistic study so we don’t no why but it is possible that acetaminophen blocks renal prostaglandin synthesis just like NSAIDs do.
Take a look at NephJC’s discussion as well as the original paper.
Riesgo de Hipertensión en el Donante Vivo de Riñón - El Resumen Visual
Risk of hypertension post living kidney donation - The Visual Abstract
The Balance of Giving: Understanding Risks for Living Kidney Donors
PRAECISely Predicting Preeclampsia
🤔 Self managed BP control after pregnancy
Long-Term Blood Pressure Control After Hypertensive Pregnancy Following Physician-Optimized Self-Management: The POP-HT Randomized Clinical Trial (Kitt, JAMA 2023)
✏️ Salt reduction still lowers BP
Effect of Dietary Sodium on Blood Pressure: A Crossover Trial (Gupta, JAMA 2023)
We know reducing sodium intake lowers blood pressure (BP), but what is truly the effect in those with normal BP versus high BP? Those taking BP meds versus those who do not? In the Coronary Artery Risk Development in Young Adults (CARDIA)–SSBP trial (Gupta et al, JAMA 2023), the investigators enrolled 213 individuals either with normal BP or not, and either on BP meds with controlled or uncontrolled hypertension. They crossed over from the usual diet to low sodium (diet with 500 mg i.e. ~ 25 mmol sodium) and high sodium (with 2 bouillon packets, each containing 1100 mg of sodium added to the usual diet). The low sodium diet did result in lower BP in all subgroups, by about 5 - 6 mmHg SBP in the normotensive/controlled hypertension subgroups to about 9 - 190 mmHg SBP in the uncontrolled/untreated hypertension subgroups. Though the authors say these are not significantly different based on interaction p values, the subgroups are woefully underpowered to say that. Note that diet allocation was on alternate days, so this was not a randomized trial. Additionally - despite being provided food and daily phone calls, people on low sodium couldn’t stick to the provided saltless diet (24 hour urine sodium 1.7g rather than 0.5 g) and even the high sodium group couldn’t stomach the extra 2.2g bouillon (24 hour urine sodium went up from 4.6 to 5.5 rather than expected 6.8 g/day). So, an extremely low sodium diet does lower BP a bit, but it’s hard to achieve even if you are provided the food. Salt substitutes are so much more pragmatic!
Swapnil Hiremath