#NephJC Chat
Tuesday October 15 9 pm Eastern
Wednesday October 16 9pm Indian Standard Time
Wednesday October 16 9pm British Summer Time
Clin J Am Soc Nephrol. 2019 Jun 7;14(6):882-893. doi: 10.2215/CJN.11590918. Epub 2019 May 23.Paperpile
Evolution Over Time of Volume Status and PD-Related Practice Patterns in an Incident Peritoneal Dialysis Cohort.
Van Biesen W, Verger C, Heaf J, Vrtovsnik F, Britto ZML, Do JY, Prieto-Velasco M, Martínez JP, Crepaldi C, De Los Ríos T, Gauly A, Ihle K, Ronco C; IPOD-PD Study Group.
PMID: 31123180 Full Text at CJASN
Patient Voice, by Shari Gilford, in CJASN
Introduction
Achieving euvolemia is one of the goals of adequate dialysis and continues to be challenging. Volume overload is associated with worse quality of life, cardiovascular disease and mortality.
In hemodialysis patients, several large and international cohort studies have shown that
incident and sustained volume overload, measured by objective methods, increase mortality in a cohort study of hemodialysis patients
various methods of volume assessment and subsequent active management of patient’s dry weight improves survival in hemodialysis patients
greater fluid overload and lower interdialytic weight gain are independently associated with mortality in hemodialysis patients
Several studies have identified a similar problem in prevalent peritoneal dialysis (PD) patients as well. This was covered in #NephMadness last year (though staying true, Scott Brimble disagreed on the importance of volume).
Prevalent patients on CAPD had symptomatic fluid retention based on clinical signs in 25% of PD patients. This was associated with increased hospitalization.
In a European cohort, assessed by body composition monitor (BCM) or bioimpedance analysis (BIA), more than 25% of prevalent PD patients had severe volume overload.
In a Chinese study of prevalent CAPD patients, overhydration was associated with an increased cardiac event rate at 1-year.
The present Initiative for Patient Outcomes in Dialysis - Peritoneal Dialysis (IPOD -PD) is an international multi-center project to study incident PD patients and their outcomes.
Volume Measurement in Dialysis
The traditional clinical exam for volume status is subjective and lacks sensitivity in detecting volume overload. Several methods of volume assessment are now increasingly used to support clinical observations in dialysis patients. Bioimpedance spectroscopy is a newer method of volume assessment where electrodes are placed on the skin and the electrical resistance between them is measured. Different tissues (blood, muscle, fat etc…) have different resistance, so the user can determine relative body composition (fat vs lean tissue) as well as intracellular vs extracellular water. Bioimpedance offers a an objective and quantitative way of characterizing volume status. In a meta-analysis published in 2017, the use of bioimpedance measurement to target dry weight in dialysis patients did not improve mortality, however, it did improve blood pressure and fluid overload state.
Rationale
Identifying dialysis prescriptions and patient characteristics associated with improved volume status may help identify better practices to help control volume status in dialysis patients. Active management of volume status may help in preventing technique failure and improve survival, this needs to be balanced against the potential for a faster decline in a patient’s residual renal function (RRF) and membrane degradation.
The authors of the IPOD-PD study aimed to characterize the volume status in a cohort of incident peritoneal dialysis population prior to starting dialysis with long term follow up of the volume status and patient-relevant outcomes.
The Study
The purpose of this international, prospective, multi-centric study was to determine how a cohort of incident peritoneal dialysis patients' volume status changed over time and to identify associations of any factors (PD prescription, diuretic use, co-morbidities etc…) associated with relative volume status.
Participants
Inclusion Criteria
Consecutive peritoneal dialysis patients over 18 years
Incident patients who chose peritoneal dialysis
Able to have bioimpedance spectroscopy measured
Exclusion criteria
Difficulty in conducting bioimpedance spectroscopy (metal implants or joints, amputations)
Pregnancy
Current treatment with hemodialysis
Study Procedures
Fresenius Body Composition Monitor (BCM) (which uses bioimpedance spectroscopy) measured the total, extracellular and intracellular water in patients. Calculations based on formulas derived in the past were used to estimate the relative amounts of adipose tissue, lean tissue and volume status of each patient.
Volume overload is the difference between the patient's extracellular volume and expected euvolemic tissue water (adipose + lean tissue). It can be quantified as the difference in liters (absolute) or as a percentage of extracellular volume (relative, sometimes described as ‘Rel FO’ in the paper). Patients were considered volume-depleted or volume overloaded when the relative fluid volume was below the 10th percentile or above the 90th percentile respectively (±7% relative volume overload.)
Baseline values including the BCM readings, PD prescription, clinical and laboratory data were collected at the start of PD therapy. The same values were again recorded at 1 and 3 months from the start date and every 3 months thereafter until the end of follow up.
Physicians were free to make changes to the PD prescription based on the BCM readings.
Analysis
This is an observational study with many exploratory analyses done, so no formal sample size estimation was done.
Volume overload is defined differently in the study at different places. For the analysis of volume overload and death, it was dichotomized at > 17.3% volume overload (not 7% as mentioned above) - though this analysis was using the competing risk method accounting for transition to HD and transplant as competing risks, and censoring drop out for other reasons.
In table 1 below, moderate refers to volume > 7% but less than 17.3% and severe to > 17.3%.
Funding
The study has been funded by Fresenius Medical Care Deutschland GmbH and Fresenius Medical Care Asia Pacific Ltd. Some of the authors are Fresenius employees.
Results
Participants
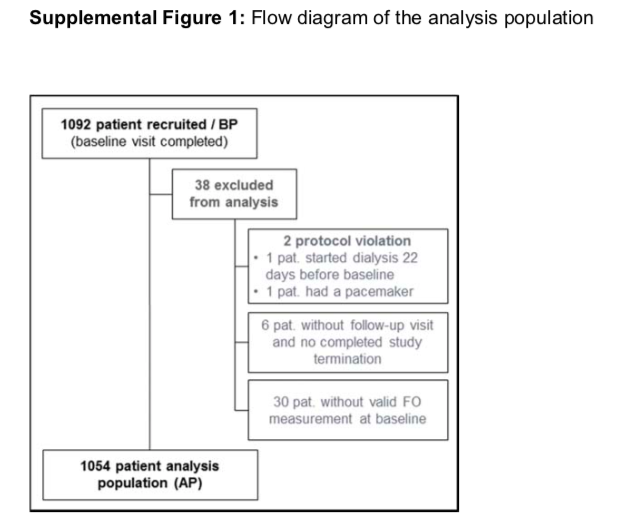
1092 patients were recruited from 135 centers in 28 countries in Western Europe, Middle East, Asia Pacific and Latin America.
The final analysis included 1054 participants.
supp figure 1 from Van Biesen et al, CJASN 2019
At baseline, not surprisingly, the majority of patients (57%) had moderate to severe volume overload. These patients also tended to have a higher frequency of diabetes and diabetic kidney disease, required more diuretics and had high or high average membrane transport type.
Table 1 from Van Biesen et al, CJASN 2019
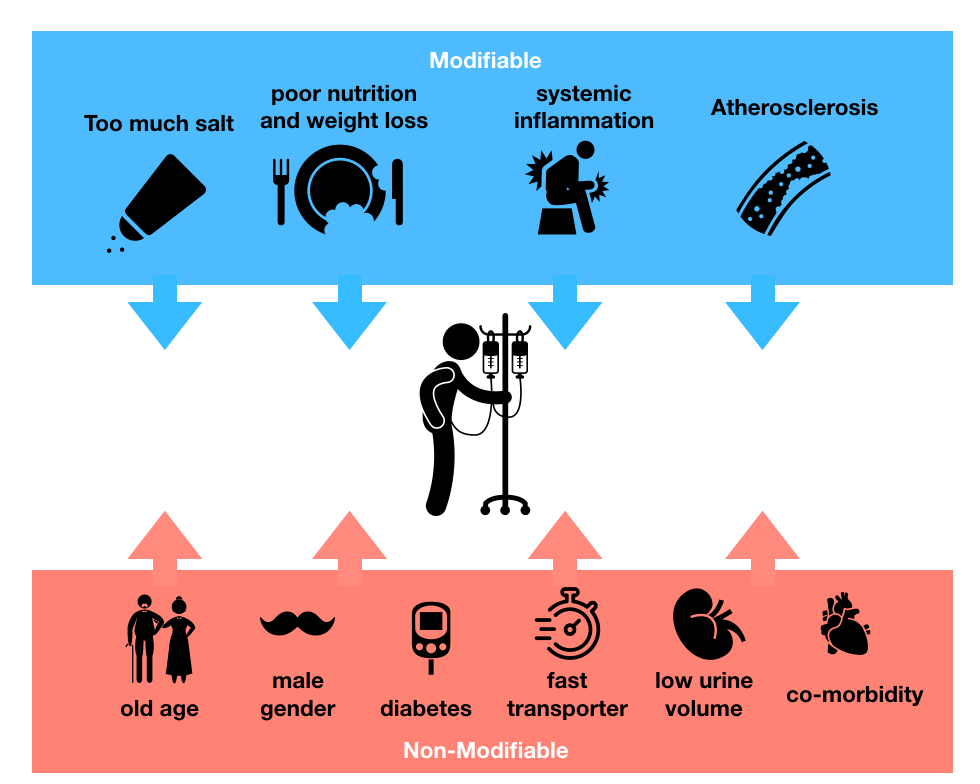
This is not surprising or new - see this figure from NephMadness, based on a review paper from Kim and Van Biesen:
However, nearly a third of the patient population did not have their transport studies done in the first 6 months. The vast majority of patients used biocompatible fluids which are commonly used in Europe.
Seventy-four percent of patients dropped out cumulatively over 3 years, so watch the numbers in the results - they pertain only to patients who remained on PD. 23% of them had (presumably) technique failure and transitioned to HD; 13% died, and 22% transitioned to transplant. The remaining 6% dropped out for other causes - it is not stated whether they remained on PD (presumably yes, if they didn’t die, get transplanted or went to HD) and were lost to follow up or recovered.
PD Practice Patterns
While most patients started on CAPD, there was a marked variation in the uptake of both automated PD (APD) and the use of polyglucose (i.e. icodextrin) depending on the regions.
Nearly 50% of the participants from western Europe were on APD by 12 months while these numbers were much lower for the other participating regions.
Figure 1 from Van Biesen et al, CJASN 2019
Similarly, the use of polyglucose (presumably icodextrin) and hypertonic solutions was far higher in the western European populations as compared to the other regions, where the use of hypertonic solutions was very high with a small uptake of icodextrin.
This seems to be a particularly important observation as a recent Cochrane review has shown that the use of polyglucose/icodextrin improved fluid removal in PD patients and reduced the rate of uncontrolled fluid overload by 70%.
Volume Status
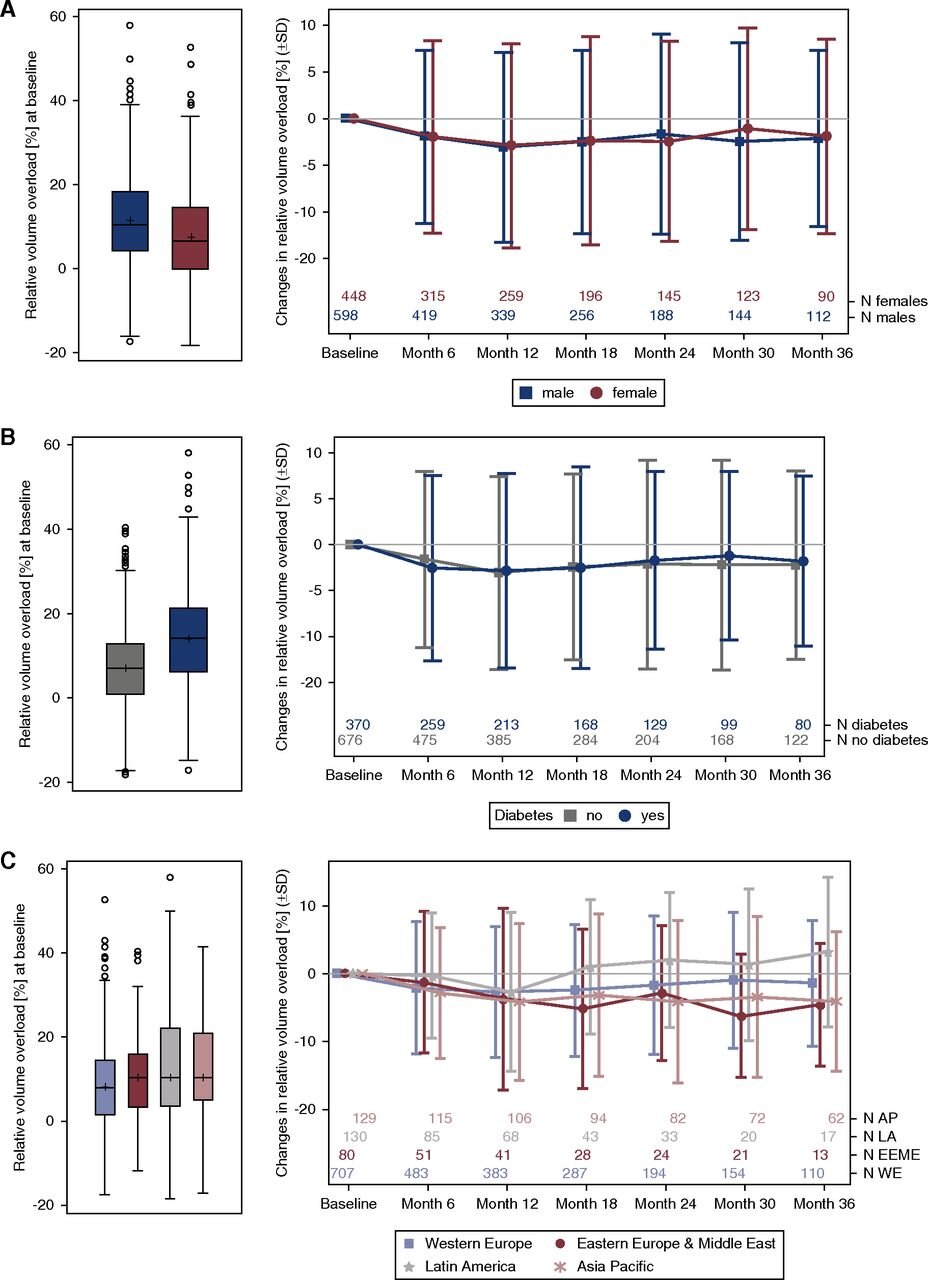
Volume overload was higher in men and in patients with diabetes at all time points. Mean volume overload was 1.9 ± 2.3 L at the start but reduced to 1.2 ± 1.8L at 12 months and then was fairly constant for the rest of the follow-up period. This was true for all regions except Latin America where the volume control worsened over the 3 years of follow up. However, see the numbers of the patients decrease over time at the bottom of the figures in the right hand panels.
Figure 2 from Van Biesen et al CJASN 2019
Relative volume overload at baseline (left panel) and mean change during the study (right panel) by (A) sex, (B) diabetes status, and (C) region. The Δ of relative volume overload/depletion in percent points was calculated for each patient and visit (baseline, month 1, month 3, month 6, and so on, until month 36) as the absolute difference between relative volume overload or depletion at the respective visit and at baseline. The plots show the interquartile range (IQR; box), mean (cross), median (line), minimum and maximum value within the IQR±1.5 IQR (whiskers), and outliers (circles). AP, Asia Pacific; LA. Latin America; EEME, Eastern Europe & Middle East; WE, Western Europe.
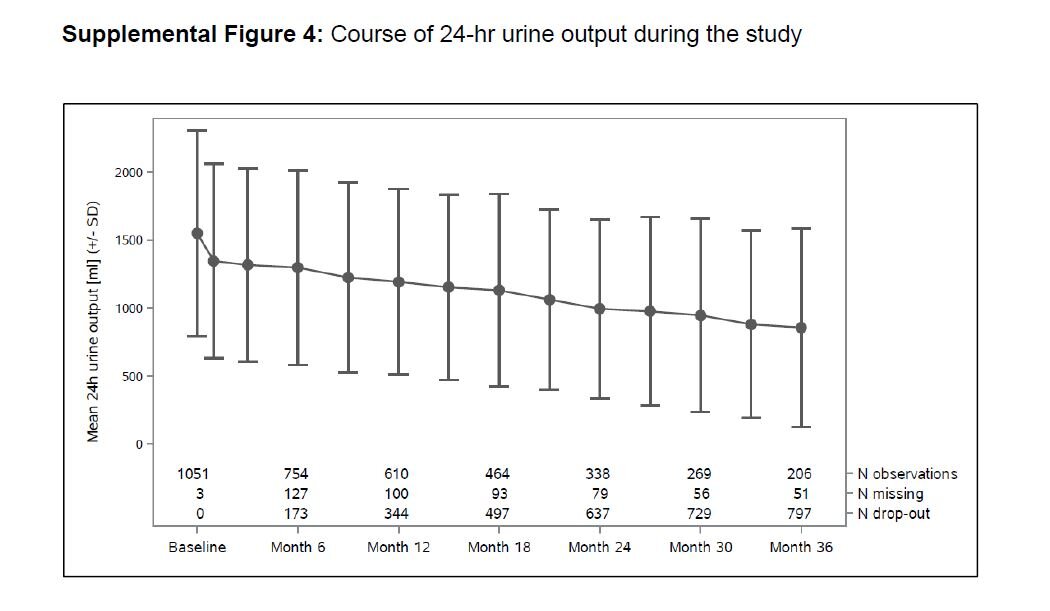
Over time, as expected, residual function declined as seen in the figure below. Hence the use of higher concentration of fluids and polyglucose, stabilized or improved volume status despite the loss of residual function (amongst the survivors).
Supp figure 4 from Van Biesen et al, CJASN 2019
Time to Death
The study identified a relative volume overload of >17.3% (or > 75th percentile) at 1 month was associated with greater mortality - HR 1.59 (95% CI 1.08 - 2.33; p = 0.02)
Figure 4 from Van Biesen et al, CJASN 2019
Cumulative incidence of death by volume status 1 month after initiating PD, adjusted for competing risks of transfer to HD and transplantation in participants with relative volume overload >17.3% versus ≤17.3% for a participant with median age, no diabetes, and no cardiovascular disease.
Discussion
This is the largest international cohort study in incident PD patients and informs the volume status of the incident patient and its course over 3 years of follow-up in various regions. This study confirms the association of mortality over 3 years, among incident PD patients with substantial volume overload (>17.3%) when measured objectively using the BCM technique.
There is an oft-repeated statement about PD patients, regarding their perpetual fluid expanded state however, this study clearly identifies that this fluid overload is present at the start and tended to decrease slightly over the first year. However, this does not account for the fact that many patients underwent transition to HD, or died over the period of follow up - and this change is hence based on outcomes in the survivors.
Male sex, diabetes and fast transporter status were risk factors associated with volume overload.
Interestingly, the international nature of the study was helpful in questioning some accepted wisdom in PD world, namely - higher glucose concentration or icodextrin like fluids are needed to achieve a state of euvolemia - this study claims that this may not be true. The patients in the Asia Pacific who used minimal hypertonic solutions were as well controlled, on the basis of BCM, as patients in Latin America who used a larger quantity of hypertonic solutions and polyglucose. It is hard to draw any conclusions, since, as the authors state, practice patterns vary - and so does availability of solutions across the world. However, perhaps a more important outcome would have been the association of a clinically important outcome (eg technique failure, or mortality, not just BCM numbers) with the hypertonic solutions and polyglucose - stratified by region. Also note that polyglucose, aka icodextrin, is manufactured by Baxter, and this study is funded by Fresenius.
Another common perception in PD is that fast transporters on PD will always be fluid overloaded - again this study helps us understand that these patients possibly were volume expanded at the start and there may be other factors in play.
Are there simpler ways of managing volume in PD patients - salt and water restriction, more diuretics (as discussed in this NephMadness commentary) ? How did that change over time in this study? The center effect is another factor that plays a role, affecting not just peritonitis outcomes, but technique failure as well. Can that be clearly accounted for?
It would be interesting to see how this study would change using the traditional exam instead. Would the amount of clinically detectable volume overload at baseline decrease? What does a typical peritoneal dialysis patient that has 17% relative volume overload look like, to a panel of clinicians? Would the majority of them agree that this represents "severely volume overloaded" as described in this study? Bioimpedance spectroscopy is not commonplace, but if it is able to detect subclinical volume overload that can be intervened upon, perhaps its use may become more widely adopted. These measurements rely on assessment of lean tissue and changes in the lean tissue mass/ nutritional state may also play an important role in patient outcomes. However, this study is not a trial. We need trial data to show that bioimpedance spectroscopy based volume assessment versus traditional assessment results in any change in outcomes.
Summary by Derian Lai
Nephrology fellow, University of Colorado
NSMC Intern, Class of 2019