#NephJC Chat
Tuesday August 21 9 pm Eastern
Wednesday August 22 8 pm BST, 12 noon Pacific
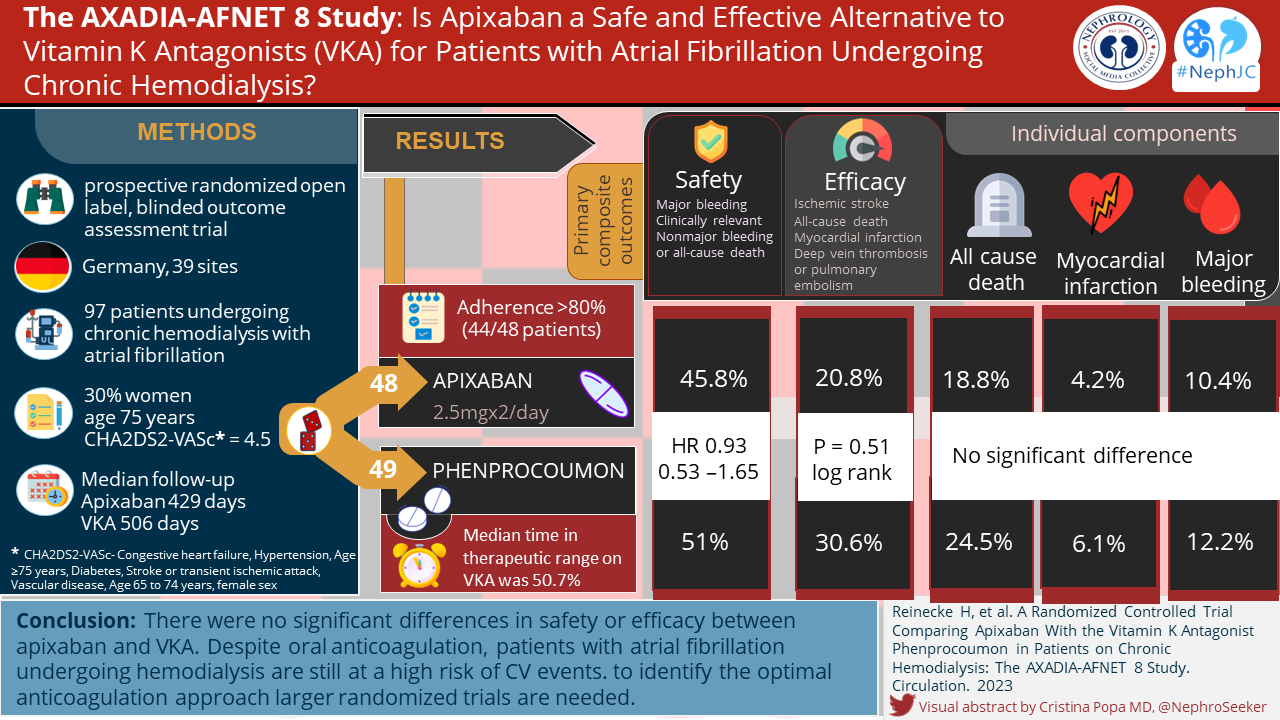
Circulation. 2018 Jun 28. pii: CIRCULATIONAHA.118.035418. doi: 10.1161/CIRCULATIONAHA.118.035418. [Epub ahead of print]
Outcomes Associated with Apixaban Use in End-Stage Kidney Disease Patients with Atrial Fibrillation in the United States.
Konstantinos C. Siontis, Xiaosong Zhang, Ashley Eckard, Nicole Bhave, Doug E. Schaubel, Kevin He, Anca Tilea, Austin G. Stack, Rajesh Balkrishnan, Xiaoxi Yao, Peter A. Noseworthy, Nilay D. Shah, Rajiv Saran, Brahmajee K. Nallamothu.
PMID: 29954737 Full Text at Circulation
Introduction
Anticoagulation in dialysis patients is a bit of a headache. Soon after I started training in Nephrology I came across a dialysis patient with atrial fibrillation (AF). They had a few other risk factors that gave them a CHADS VASC score that made them a candidate for anticoagulation...in a non-dialysis patient.
“Should we start warfarin?” I asked my consultant.
“Good question. Why don’t you look into it.” they replied.
Enthusiastically I dived into what could only be described as a minefield of retrospective evidence and expert opinions. Patients with ESKD are at high risk of stroke . Patients with AF and ESKD are at even higher risk . Unfortunately, they were also at high risk of bleeding so the benefit usually seen with anticoagulation is not as clear in ESKD.
Warfarin was the only anticoagulant realistically available to use in our dialysis patient and we didn’t have compelling evidence pointing us to the best answer. It seemed we couldn’t win.
Do we note AF and then ignore it while praying the patient does not develop a stroke.
Or note the AF, start warfarin and worry about the patient getting a bleed.
Or note AF, decide the patient is too high risk of bleeding and don’t start it. Later the patient develops a venous thrombosis and starts warfarin anyways.
Or do we decide that a patient with new AF and a previous stroke would benefit from some warfarin. Start it and then watch in horror as they develop calciphylaxis.
You couldn’t win. Added to this was having INR monitoring done at dialysis, inconsistent prescribing, polypharmacy and aspirin use. It is a recipe for disaster.
This new study shines some evidence on a new option when we get stuck between atrial fib, warfarin, and a hard place.
The big trials done with DOACs have excluded patients with ESKD. Some data have suggested that rivaroxaban and dabigatran use in dialysis patients is associated with adverse outcomes. There are some dosing recommendations on apixaban in dialysis patients but it was based on pharmacokinetic data. The FDA approved apixaban use in haemodialysis patients without empiric patient data. There was zero data on how apixaban use in ESKD translated into clinical outcomes in dialysis patients. Did it prevent strokes as well as warfarin? Was it better? Worse? More side effects?
The Study
Methods
This was a retrospective cohort study on Medicare beneficiaries done using USRDS data.
It looked at patients with ESKD on dialysis (HD and PD) with AF diagnosed within the last year and a new prescription for an anticoagulant between October 2010 and December 2015. Those with ‘Valvular AF’ were excluded. This study looked at apixaban versus warfarin. Although data was collected on the small number of patients prescribed dabigatran or rivaroxaban this was excluded from further analysis.
Patients were followed until study end, death, or censoring. Censoring occurred if the patient:
Discontinued or switched their anticoagulant
Stopped dialysis due to improvement in kidney function or transplant
Loss of Medicare
Development of valvular AF
The outcomes were:
stroke or systemic embolism
Major bleeding: cranial site (e.g. intracranial), requires transfusion, associated with a cardiac arrest or death
GI bleeding
Intracranial bleeding
Death
Apixaban and warfarin patients were matched in a 1: 3 ratio. The groups were matched using the prognostic score, which the authors call as the outcome based equivalent of propensity scores.
Differences in event free survival between the groups was assessed using Kaplan-Meier curves. Hazard ratios and 95% confidence intervals were derived from Cox regression analyses.
Results
The study population consisted of 25,523 patients (45.7% women; age 68.2±11.9 years).
2,351 patients on apixaban
23,172 patients on warfarin
An annual increase in apixaban prescriptions was observed following its marketing approval in the end of 2012. By 2015 26.6% of new anticoagulant prescriptions were for apixaban. (Figure 1)
8,461 (33.2%) patients had a prior CVA and 2,536 (9.9%) patients had prior major bleeding.
The mean CHA2DS2VASc score was 5.2±1.8.
Figure 1. Trends in new oral anticoagulant prescriptions in AF patients with ESKD on dialysis in the United States (2010-2015)
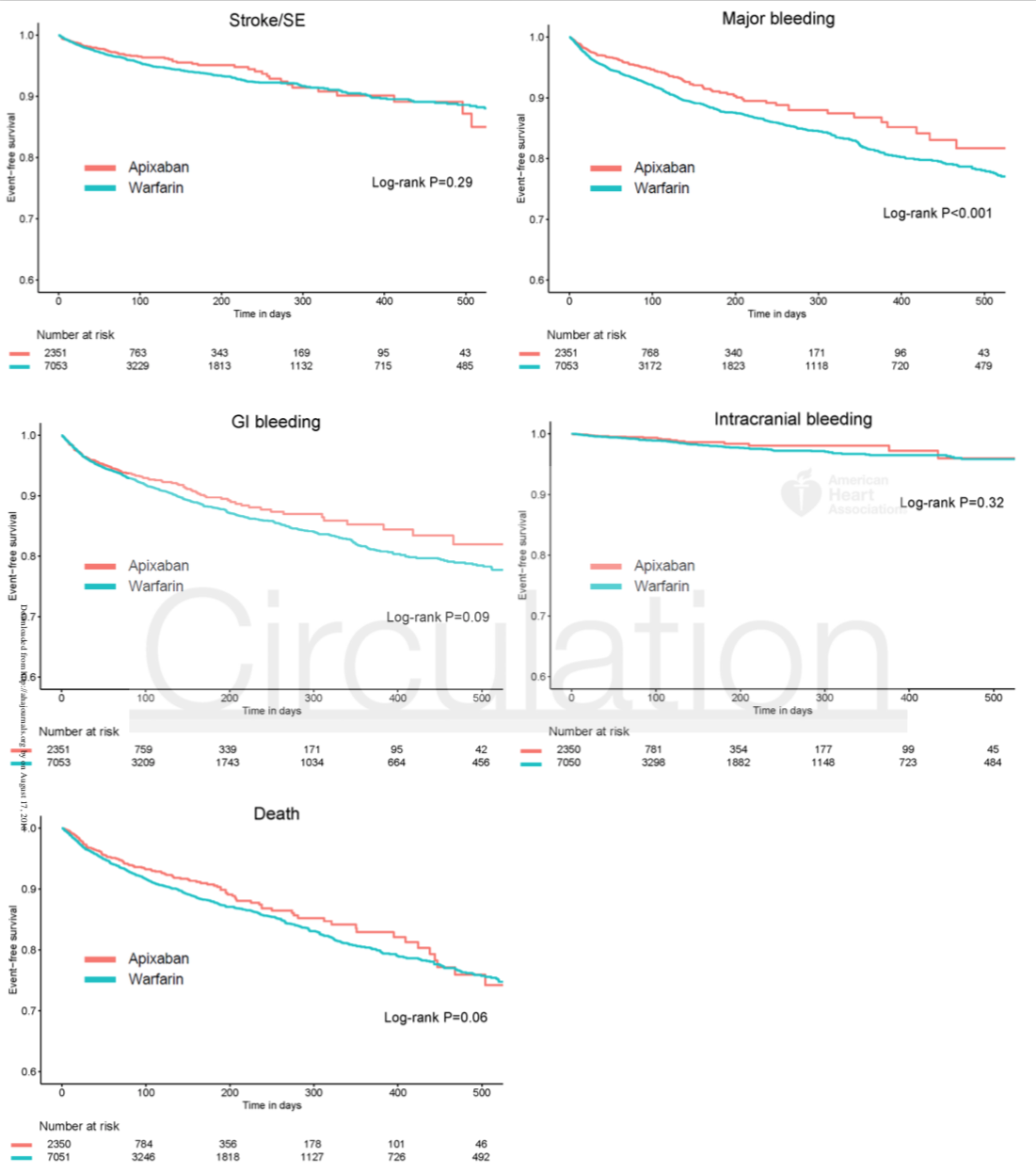
The event rates for stroke/SE were 12.4 and 11.8 per 100 patient-years for the apixaban and warfarin groups, respectively, with no difference in survival free of stroke/SE between groups (HR 0.88, 95% CI 0.69-1.12; P=0.29).
Apixaban was associated with a significantly lower risk of major bleeding with 19.7 versus 22.9 per 100 patient years (HR 0.72, 95% CI 0.59-0.87; P<0.001). No significant difference was noted between the groups for intracranial bleeding. Apixaban was not associated with reduced mortality (HR 0.85, 95% CI 0.71-1.01; P=0.06).
Figure 2: Kaplan-Meier survival curves for the apixaban group and a prognostic-score matched warfarin cohort for stroke/SE, major bleeding, GI bleeding, intracranial bleeding and death.
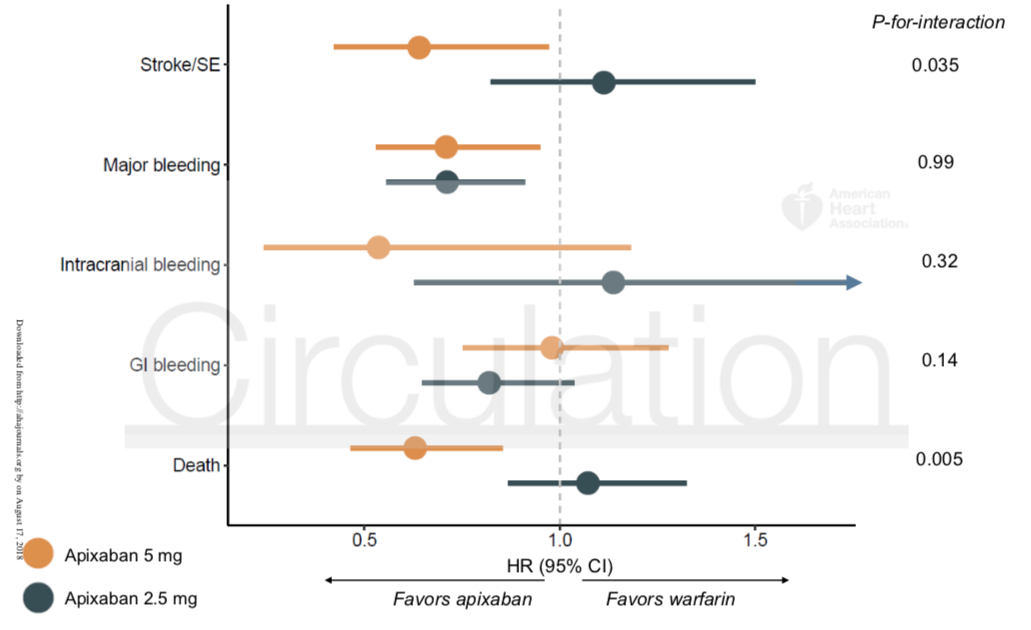
In sensitivity analyses, 5 mg apixaban bid (n=1,034) was associated with lower risks of stroke and death compared with either 2.5 mg bid apixaban or warfarin.
Figure 3: Association estimates from dose-specific comparisons of apixaban versus warfarin. Hazard ratios and 95% confidence intervals are derived from Cox regression analyses in prognostic score-matched cohorts of apixaban 2.5 mg and apixaban 5 mg doses to warfarin
In both the apixaban and warfarin cohorts, the rates of censoring due to expiration of the prescription or >30-day gap between prescriptions were high, (62.4% and 72.5%, respectively. The majority of these censorings occurred in the first 12 months after the prescription (60.9% and 66.4%, respectively), and another 5.6% and 8.9% of patients in the apixaban and warfarin groups, died in the first 12 months.
Discussion
Strengths:
This was a large study looking at 25,000 patients including >2000 on apixaban. it’s the first study looking at the effectiveness and safety of apixaban in dialysis patients. This study included a wide range of patient demographics and ESKD characteristics and included both HD and PD patients.
Weaknesses
This uses observational data as opposed to being a RCT. There was a high percentage of anticoagulation discontinuation in both groups. Both groups had a high rate of major bleeding, the intracranial bleed rate was much higher than in non ESKD patients. There is no non-treatment group. The full utility and risk benefit of anticoagulation in dialysis patients is not fully understood. Aspirin use was not captured.
What can we learn from this study?
Bearing in mind that this is an observational study, and that there was a high rate of anticoagulation discontinuation and of bleeds in both groups, I think this study is a useful one. I am reassured that apixaban is possibly just as good as warfarin in preventing stroke in ESKD patients and actually is associated with a lower risk of bleeding. Given the available data I still may not reach for apixaban in the first instance but it’s good to know we have a safe and effective option if we need it.
Will we ever get better data? There are three ongoing trials in this area:
The RENAL-AF trial of apixaban (5 mg bid; 2.5 mg bid in select patients) versus warfarin, with N = 762, in ESRD patients
AXADIA trial of apixaban (2.5 mg bid) vs Phenprocoumon (a Vit K antagonist like warfarin), with N = 222, in ESRD patients
the AVKDIAL, which is the largest one of these three, with N = 855 of a vit K antagonist vs no treatment, in ESRD patients
These will definitely provide more robust data for the future.
And given the complexity of anticoagulation in dialysis, we’ll need it!
Summary by Sarah Gleeson, nephrology trainee, Auckland
NSMC intern, class of 2018