#NephJC Chat
Tuesday Feb 28th 9 pm Eastern
Wednesday March 1st 8 pm GMT, 12 noon Pacific
JAMA Intern Med. 2017 Feb 6. doi: 10.1001/jamainternmed.2016.8865. [Epub ahead of print]
The Illness Experience of Undocumented Immigrants With End-stage Renal Disease.
Cervantes L, Fischer S, Berlinger N, Zabalaga M, Camacho C, Linas S, Ortega D.
PMID: 28166331
Free Access (courtesy JAMA Int Med): Link (expires March 3rd 2017)
Commentary in JAMA Int Med
Related article on Hospice Access for undocumented immigrants in same issue
Commentary from @MethodsmanMD, Perry Wilson:
Post on the RFN from Nate Hellman
A New York Times article on this issue (from 2010)
Introduction
Francisco is an undocumented immigrant who works as a landscaper and has been living in the U.S. for the last 35 years. He regularly sees a physician and pays in cash for his clinics visits and medications; he was diagnosed with CKD 8 years ago, but now is approaching ESRD. His extended family (some of them living legally in the US) are potential living kidney donors and are willing to undergo testing. Francisco does not want to give up and he wants to continue being productive and provide for his family. His clients have offered him monetary assistance . What are his options? Should we wait until he needs urgent hemodialysis? Should we provide a referral for dialysis, education, AVF or kidney transplant evaluation? Should Francisco return to his country of origin? Should he move to a more “undocumented people-friendly state”? Can he buy health insurance?
The Emergency Medical Treatment & Labor Act (EMTALA) was enacted in 1986 to “ensure public access to emergency services, regardless of ability to pay…”; however, the Patient Protection and Affordable Care Act (ACA, iaka Obamacare) does not include access to healthcare for undocumented immigrants.
A survey in 2009 among Nephrologists reported that 642 nephrologists (out of 990 who responded), have provided dialysis services to undocumented patients and 67% of those nephrologists did it as outpatient and 59% provided emergency dialysis care. The majority felt that reimbursement was inadequate. Furthermore, there is a misconception that undocumented patients come to the U.S for health benefits; the latest literature reveals that in fact, undocumented immigrants contribute less to health care costs and use fewer medical services. Surprisingly, in a small survey in 2012 among AJKDblog readers, close to 58% of respondents, did not support kidney transplantation.
Currently, in the United States there are approximately 6,500 undocumented immigrants needing a form of renal replacement therapy, mainly hemodialysis. I am unaware of any data of patients undergoing peritoneal dialysis, which would be far more cost effective. These patients, depending on the state in which they live, have to either have insurance coverage to undergo scheduled hemodialysis or must wait to develop fluid overload symptoms in order to meet criteria to be admitted for emergent hemodialysis. The cost for receiving emergent hemodialysis ranges from $285,00 to 400,000 across the U.S. This present qualitative study of 20 undocumented hemodialysis patients from Latin America, living in the US for at least 4.2 years, for the first time explored the feelings of undocumented patients undergoing urgent hemodialysis. According to this previous report, there are approximately 6,500 undocumented immigrants on hemodialysis. This issue is not exclusive to the United States, but also to first world countries that receive large numbers of immigrants.
Study Design:
- Single center study in Denver, Colorado, from July 1 to December 2015
- 20 semistructured interviews with undocumented Hispanic patients requiring hemodialysis
- Patients signed informed consent and received financial compensation.
- Professional Interpreters were used at the time of interview.
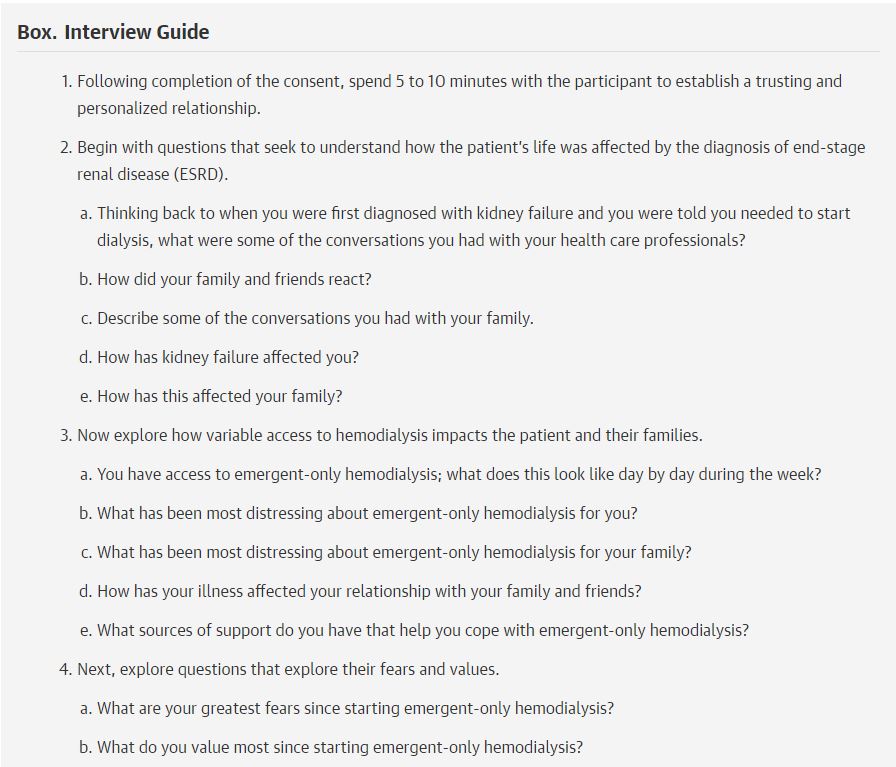
Box from Cervantes et al, JAMA IM 2017
Inclusion Criteria
- Patient needing urgent hemodialysis (with no access to schedule HD)
- Arteriovenous fistula
- Admission criteria for urgent hemodialysis: potassium >5.2 mEq/L, bicarbonate less than 15, hypoxia (<90%), uremic symptoms (confusion, dyspnea, nausea, vomiting, altered mental status)
- Patients were admitted for two nights; received hemodialysis two days in a row (When available).
Exclusion Criteria
- Patients lacking decisional capacity
Results:
Table 1 from Cervantes et al, JAMA IM 2017
After the questionnaire was performed, answers were split in themes:
- Distressing Symptom Burden and Unpredictable Access to Emergent-Only Hemodialysis
- Death Anxiety Associated With Weekly Episodes of Life-Threatening Illness
- Family and Social Consequences of Accommodating Emergent-Only Hemodialysis
- Perceptions of the Health Care System
Table 2 from Cervantes et al, JAMA IM 2017
Discussion
As the authors suggest, this is one of the first studies that focus on the psychological and physical challenges, including near-death experiences that undocumented immigrants endure during their hemodialysis journey. I have taken care of many undocumented patients (not only Hispanics), and as a health care provider, I feel a great deal of empathy after reading the comments of the patients included in the study. As a physician, I just want to deliver the best standard of care for my patients. The best option is not always the most expensive, but the more cost effective, which sometimes happens to be the one with the best outcomes. Although this article included only 20 patients, it sheds light about the problems these patients face on a daily basis which varies according to the state in which patients reside. Even though they received substandard health care, they are still grateful with healthcare personnel.
The following States provide scheduled maintenance hemodialysis and is important for every Nephrologist to know: Arizona, Delaware, Florida, Illinois, Massachusetts, Minnesota, New York, North Carolina, Virginia, Washington and District of Columbia. Some states, like Illinois, have begun to cover (PDF link) undocumented immigrants in need of a kidney transplant as well, clearly decreasing the costs of dialysis. New York State has a similar program with certain limitations. In other states, there are safety net hospitals, which provide dialysis, amongst other services, for undocumented immigrants. Furthermore, many of these patients have a donor, but because their lack of access to health care (even if they are good transplant candidates), they are not eligible, unless they pay out-of-pocket. In fact, it has been shown that undocumented immigrants tend to have better outcomes than their U.S. counterparts.
So what would be the ideal health insurance plan for an undocumented patient? An off-exchange policy, but the ACA prohibits undocumented patients from using such a plan so changes in the Federal and State law (like California) would have to be implemented.
I found minimal limitations in the study other than those acknowledged by the authors including the use of a single center and the small sample size. I wonder if some patients declined to be in the study for fear of immigration repercussions. It would be interesting to know the experience of undocumented immigrants on scheduled hemodialysis as well. .
As the editorial suggested, small changes in local and state laws to the health care system have been enacted to include undocumented immigrants; some non-profit organizations have also stepped in, but the Medical and Nephrology Societies and Federal Government need to address the issue of undocumented immigrants living in the U.S. needing hemodialysis (or experiencing some of the catastrophic diseases) so we, as physicians, would not have to deliver substandard care or have an ethical dilemma, regardless of costs or immigrations status. The fact the these patients have to wait to develop near-death symptoms to be dialyzed, is alarming to me and should be a concern for Nephrologists and Lawmakers.
The Renal Physicians Association states: ”...health care professionals have an ethical obligation to treat the sick (including the ESRD population), and the Federal Government has an ethical responsibility to provide life-sustaining care for anyone within the U.S. borders….”
Summary written by Hector Madariaga, Nephrologist, Boston