#NephJC Chat
Tuesday April 24 9 pm EDT
Wednesday April 25 8 pm BST, 12 noon PDT
JAMA Intern Med. 2018 Apr 9. doi: 10.1001/jamainternmed.2018.0411. [Epub ahead of print]
Dialysis Initiation and Mortality Among Older Veterans With Kidney Failure Treated in Medicare vs the Department of Veterans Affairs.
Kurella Tamura M, Thomas IC, Montez-Rath ME, Kapphahn K, Desai M, Gale RC, Asch SM.
INTRODUCTION
Whether or not to commence dialysis (and if so, when to do so) in our older and frail patients remains one of the trickiest aspects of nephrology practice. On the one hand, we know that lack of adequate preparation for renal replacement therapy leading to “crash start” dialysis (i.e. poor nutritional status, inadequate vascular access, life-threatening metabolic derangements at the time of dialysis initiation) is associated with worse outcomes. But on the other hand, we have RCT data that demonstrate a lack of benefit to earlier initiation of maintenance dialysis. We also know that in some high co-morbid groups such as nursing home residents, the commencement of dialysis is highly predictive of substantial harm.
The authors of the current study postulate that factors external to the patient’s health status and preferences may influence the decision to initiate dialysis. In the U.S., veterans older than 65 years account for nearly 20% of all incident dialysis patients. Since older veterans are eligible to receive pre-ESRD nephrology care in the commercial system with Medicare as the payer or with the Veterans Administration (VA), the authors designed a natural experiment to test whether the site of pre-ESRD nephrology care is associated with more frequent dialysis initiation and higher survival in those with advanced kidney failure.
METHODS
Design and Data Sources:
Retrospective cohort study using cross-linkable data from the VA, Medicare claims, and the United States Renal Data System (USRDS), the U.S. national registry of patients receiving dialysis therapy for ESRD.
Study Population:
11,215 veterans aged 67 years or older with incident kidney failure between 2008-2011, defined as either:
Progression of CKD to a sustained eGFR < 15mL/min/1.73m2 during follow-up, or
Initiation of maintenance dialysis.
Exposure:
The study population was divided into two groups: those who received
Medicare (N=3974) vs.
VA (N=7241) pre-ESRD nephrology care
for 2 years prior to developing kidney failure. In the U.S., Medicare is the federal social insurance program that provides health insurance for people age 65 and older (as well as those who are disabled, and those getting chronic dialysis or have had a kidney transplant). Therefore, this chosen group of veterans should have had dual-eligibility to receive Medicare and/or VA health insurance coverage in the two years leading up to incident kidney failure.
Figure 1 from Kurella Tamura et al, JAMA Int Med, 2018
Primary Outcomes:
The study cohort was followed for 2 years through to 12/31/2013 for:
1. Initiation of maintenance dialysis
2. All-cause Mortality
Statistical Analysis:
In the main analysis using the entire cohort of 11,215 veterans, the authors used modified Poisson regression to determine the association between the site of pre-ESRD nephrology care (primary exposure) with dialysis treatment and death (primary outcomes).
To account for different characteristics in the two groups that may be associated with the outcomes (i.e. potential confounders), they adjusted for important variables such as demographics, co-morbidities (such as diabetes, ischemic heart disease, CHF, liver disease, malignancies, depression), number of pre-ESRD nephrology visits, rate of eGFR decline before incident kidney failure, marital status, zip code median income, urban residence, nearest VA driving distance, VA co-pay, and year of incident kidney failure.
A secondary analysis was performed using propensity score matching. This is another acceptable technique (aside from multivariable regression analysis) to account for potential differences in the two exposure groups that may be associated with outcomes. Propensity scores (i.e. the predicted probability of Medicare vs. VA care) are estimated with logistic regression models using the site of pre-ESRD care as the outcome – and all the above mentioned patient characteristics as predictors. Ultimately, patients with similar characteristics are matched in a 1:1 ratio in terms of site of pre-ESRD nephrology care, as shown in Table 1, deriving at a final propensity-matched analytic cohort size of 5932.
RESULTS:
The study population was 99% men with mean age of 79 years. The Medicare group tended to be older, more likely to be male, white, and married; and had greater barriers to VA care (farther from nearest VA, more rural, and have co-pay for VA services). These differences were accounted for in the propensity-matched analysis.
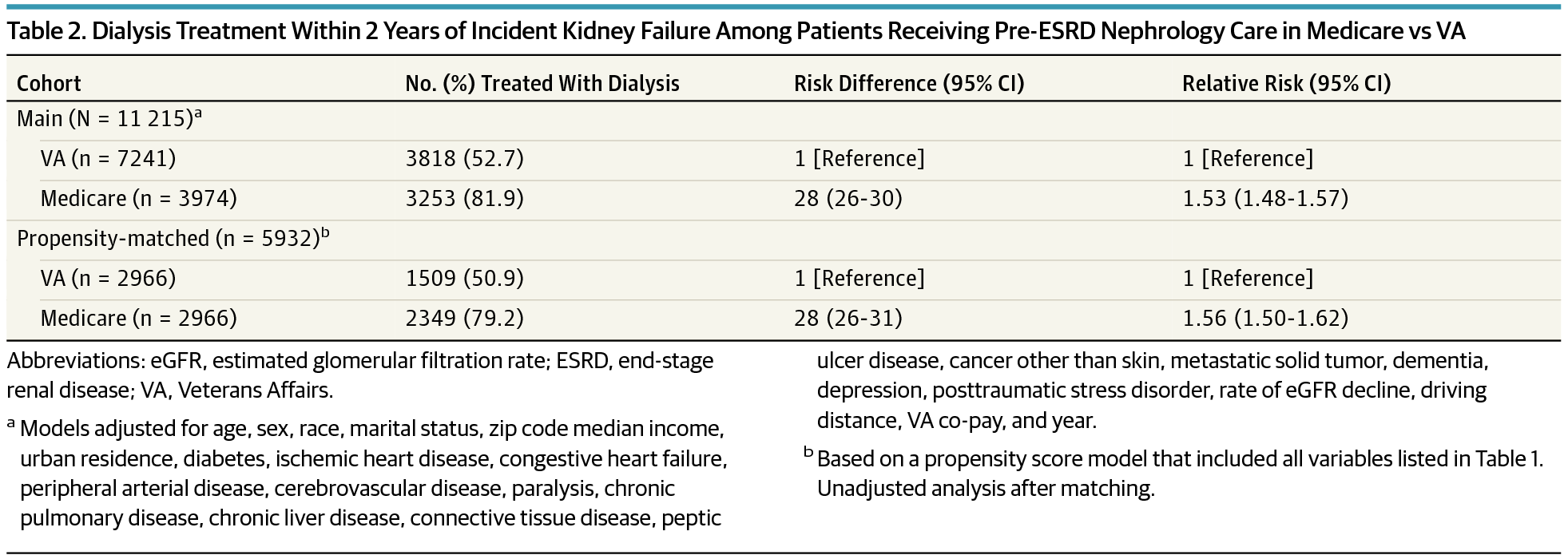
Dialysis treatment:
The frequency of commencing dialysis treatment was higher in those who received Medicare nephrology care (82%) vs. VA care (53%), conferring an adjusted risk difference of 28% (adjusted relative risk of 1.53, 95% CI 1.48-1.57). Propensity-matched analysis yielded an identical 28% higher frequency of dialysis for the Medicare group (RR 1.56, 95% CI 1.50-1.62) compared to the VA group.
Table 2 from Kurella Tamura et al, JAMA Int Med 2018
Notable patient characteristics found to be associated with differences in the likelihood of dialysis treatment between the two groups (i.e. significant interaction or effect modification between patient characteristic and the site of pre-ESRD nephrology care) include:
≥80 years old: more likely to be dialyzed if they received Medicare nephrology care (aRR 1.78, 95% CI 1.69-1.87)
Dementia: more likely to be dialyzed if they received Medicare nephrology care (aRR 1.82, 95% CI 1.63-2.01)
Metastatic cancer: more likely to be dialyzed if they received Medicare nephrology care (aRR 2.00, 9 5% CI 1.64-2.35)
Mortality:
A staggering 47% of patients died within 2 years of incident kidney failure. Most notably, there is a 5% higher frequency of death among those who received Medicare pre-ESRD care compared to those who received VA pre-ESRD care.
DISCUSSION
...higher utilization of dialysis was associated with a higher 2-year mortality...
Dialysis appears to be the default treatment modality for a majority (63%) of older veterans with incident kidney failure, with patients who received pre-ESRD nephrology care through Medicare having a 28% higher frequency of dialysis initiation compared to patients who received pre-ESRD nephrology care through the VA. This higher utilization of dialysis was associated with a higher 2-year mortality.
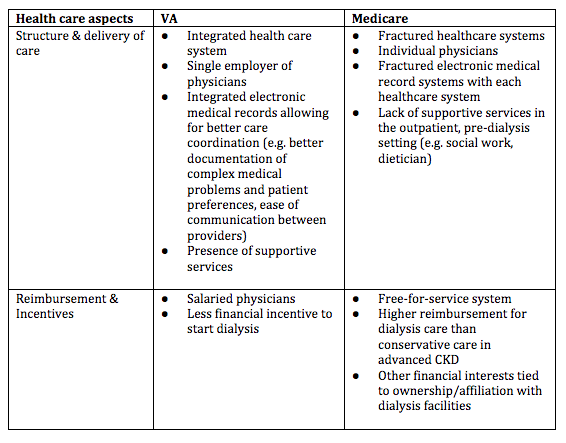
So why is there such variation in patterns of dialysis initiation among a cohort of older advanced kidney failure patients, after accounting for potential differences in characteristics within the two groups? The authors postulate that differences in how health care is structured and delivered through the VA vs. Medicare may offer plausible explanations:
Nearly half of all patients in this cohort died within 2 years of reaching incident kidney failure. This is quite sobering but not surprising to practicing nephrologists who are increasingly caring for an aging population. Older patients with advanced kidney failure have high number of co-morbidities, and the results of this study suggest that more frequent dialysis initiation does not confer a survival benefit (and may in fact, be harmful). Certain subgroups were particularly prone to dialysis initiation if they had Medicare nephrology care (vs. VA care): the very old (≥80 years), those with dementia, and those with metastatic malignancy. This suggests that inadequate counseling and (mis)informed decision-making regarding dialysis initiation among frail patients who are unlikely to benefit from dialysis.
Overall, this is an elegantly performed study with a large national sample size and rigorous statistical methods, including a secondary analysis using propensity scores to combat confounding. Limitations include: lack of generalizability to younger patients and women; possible misclassification of incident kidney failure among Medicare patients who did not initiate dialysis; and lack of data on patient preferences between the two groups.
This is not the first study that has shown higher performance of VA processes of care compared to non-VA counterparts. Recent policy changes and momentum toward expansion of veteran healthcare to non-VA, private systems may have unintended consequences if care is not carefully coordinated across systems (See NYT Op Ed by the former secretary of the Department of Veteran Affairs, David Shulkin)
One logical next step would be to tease out which aspects of VA care are responsible for these findings so that they may be potentially adapted to healthcare systems outside of the VA. From a policy standpoint, we should strive to advocate for the realignment of financial incentives so that dialysis is not inadvertently (or deliberately) started on frail, older adults who are unlikely to derive benefit from treatment (See accompanying editorial by Chen Z et al.).
Summary by Raymond Hsu, Nephrologist, San Francisco