#NephJC chat
Tuesday March 14th 9 pm Eastern
Wednesday March 15th 8 pm GMT, 12 noon Pacific
J Am Soc Nephrol. 2016 Dec 22. pii: ASN.2016070806. doi: 10.1681/ASN.2016070806. [Epub ahead of print]
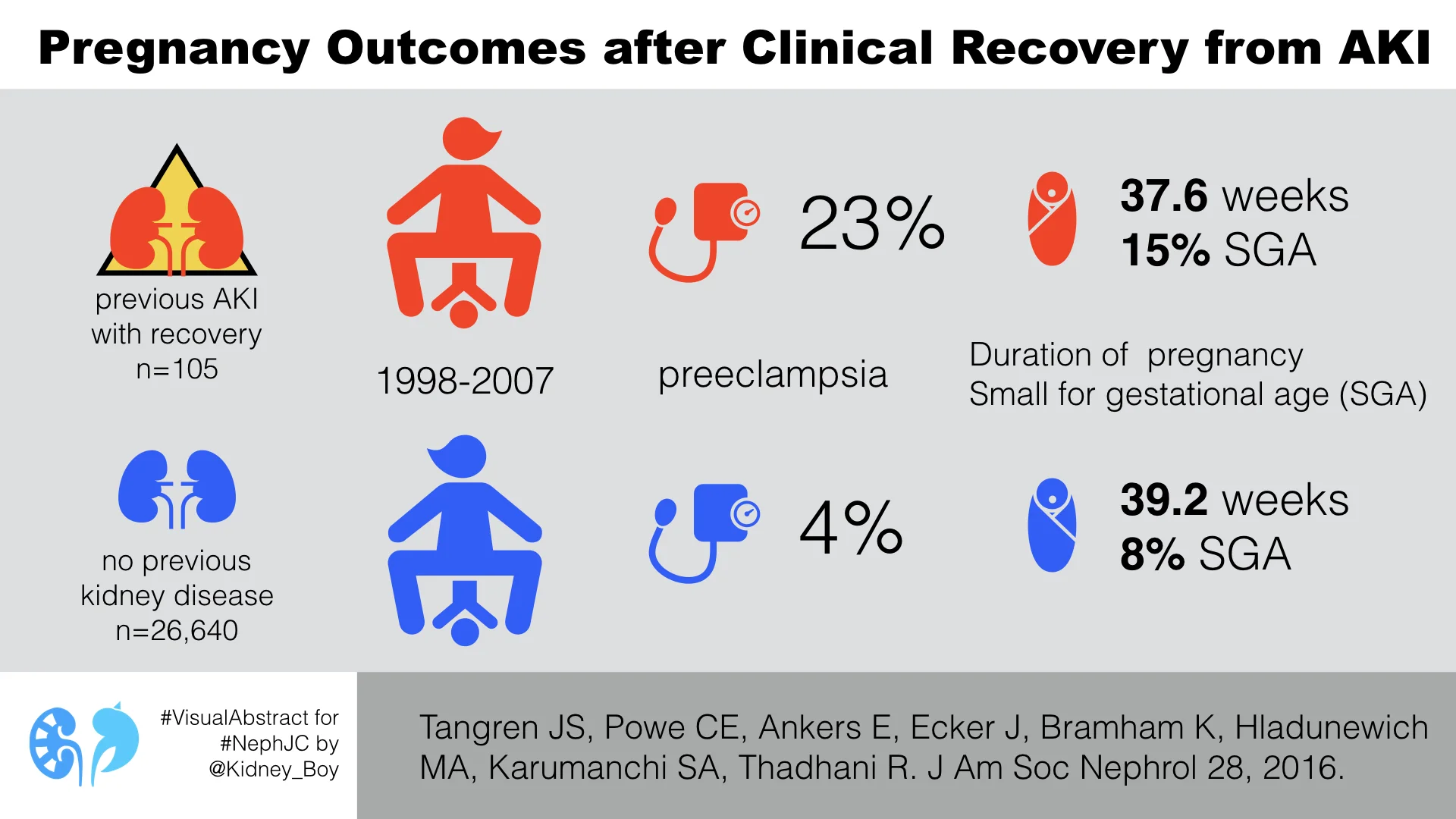
Pregnancy Outcomes after Clinical Recovery from AKI.
Tangren JS, Powe CE, Ankers E, Ecker J, Bramham K, Hladunewich MA, Karumanchi SA, Thadhani R.
PMID: 28008002
Free full text link (thanks to JASN!)
Supplemental Data PDF link
Introduction
Pregnancy is always a challenging time, not least for the kidneys. As a pregnancy progresses, the kidneys and placenta must work to meet the homeostatic demands of a developing human. For instance, GFR increases during pregnancy up to 50% above baseline levels to help meet these demands. What are the consequences for pregnancy if the kidneys have previously sustained an injury? We know that even early stage CKD leads to significantly worse outcomes in pregnancy. Furthermore, donor nephrectomy also increases the risk of preeclampsia. The link between past AKI and risk of development of CKD is well established. So the authors of this study reasoned that the subclinical renal dysfunction present after AKI, even with full clinical recovery, might increase the risk of poor outcomes in pregnancy.
Study design:
- Retrospective single centre study over 9 years.
- AKI defined solely on creatinine (rise ≥ 1.5x baseline)
- Compared maternal outcomes including preeclampsia, gestational hypertension gestational age, and Cesarean section.
- Compared fetal outcomes including birth weight, perinatal death, NICU admission, and small for gestational age.
Inclusion criteria
- Women with an episode of AKI with subsequent recovery of renal function (eGFR >90) prior to pregnancy
- Exclusion criteria
- Women with CKD (I-IV) or eGFR<90 prior to conception without a CKD diagnosis
- Multiple pregnancies
- 2+ proteinuria at the initial prenatal visit
- Presentation after 20 weeks gestation
Results
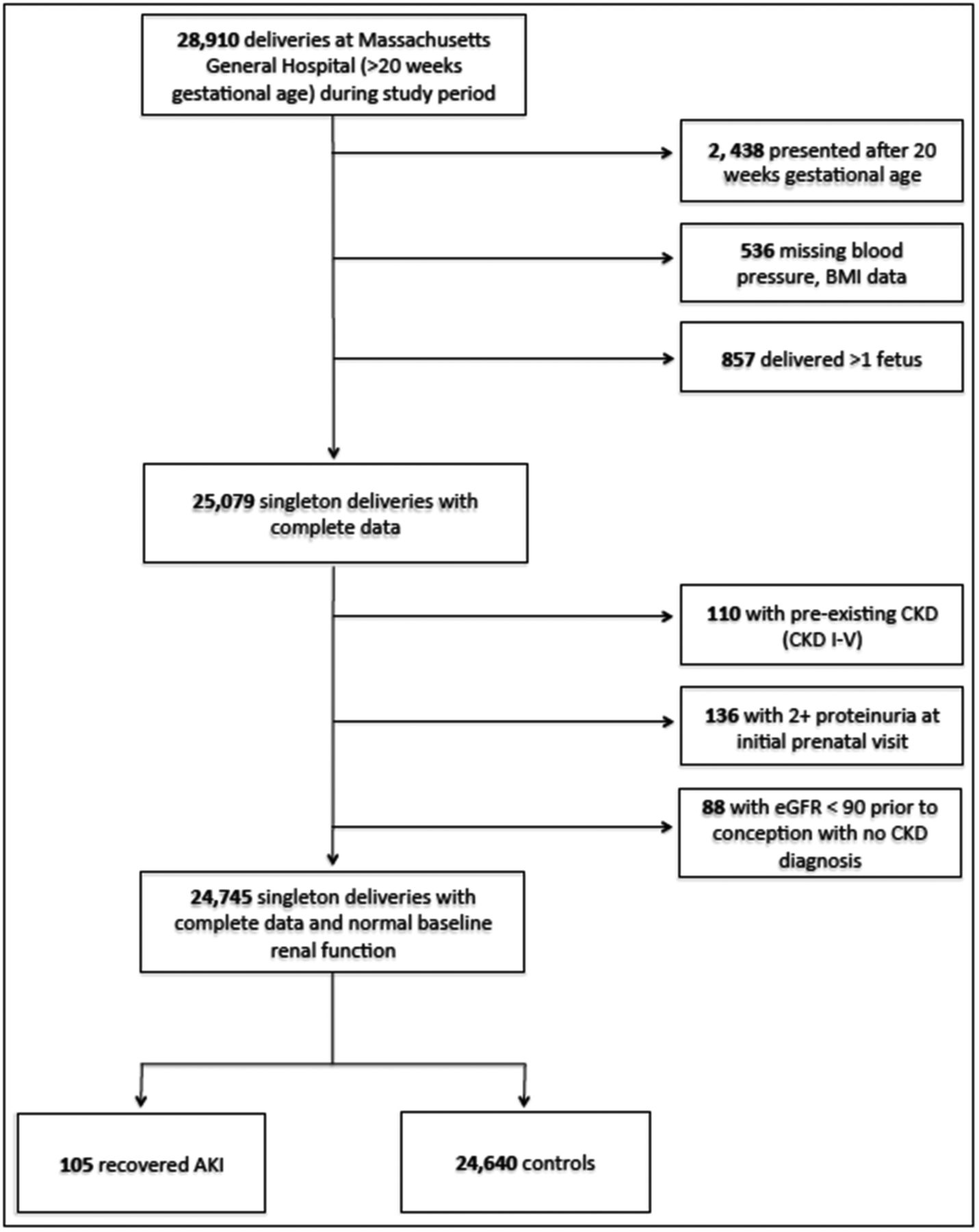
Figure 1 from Tangren et al JASN 2017
Participant characteristics
Overall, the groups were well matched with the exceptions that:
Controls were more likely to be of self-reported nonwhite race
Women with recovered AKI were more likely to be diabetic
Women with AKI prior to pregnancy experienced AKI with a range of etiologies. Most were either pre-renal injury or acute tubular necrosis (40%). Thereafter drug-induced renal injury (12%) and AKI as a result of a previous pregnancy (12%) vied for the next most common.
AKI resulting from a previous pregnancy, incorporated a range of pathologies:
- Hyperemesis gravidarum
- Pre-eclampsia or HELLP syndrome
- Obstetric haemorrhage
Women with recovered AKI were significantly more likely to have a lower gestational age at delivery and need a cesarean section. Their rates of preeclampsia were also significantly higher. Offspring of women with recovered AKI were more likely to require NICU admission, highlighting the apparent high risk nature of these pregnancies.
The authors used three analysis strategies to avoid confounding effects:
Multivariate logistic regression
After multivariate analysis, the association of recovered AKI with preeclampsia and adverse fetal outcomes persisted
Matched analysis
Matching each woman with recovered AKI to two without, by age, race, BMI, parity, diabetes status, and diastolic BP in the first trimester.
The results of this were much the same, however, the frequency of small for gestational age was not significant.
Figure 2 from Tangren et al JASN 2017
Subgroup analysIs
Past preeclampsia increases the risk of having preeclampsia with subsequent pregnancies. 12% women with recovered AKI experienced AKI as a result of pregnancy, so the authors went on to perform a subgroup analysis excluding these women. As they did not have past preeclampsia data history on all women, they also performed a subgroup analysis in nulliparous women.
They also performed subgroup analyses excluding various populations to try and dissociate the effect from other risk factors for adverse outcomes:
- Diabetes Mellitus
- Hypertension
- Obesity (BMI >30)
Figure 3 from Tangren et al JASN 2017
In all these analyses, the association with adverse pregnancy outcomes, particularly pre-eclampsia, was maintained.
Limitations
Women who previously experienced a creatinine rise of over 0.3 mg/dl over 48 hours (meeting KDIGO criteria) were not assigned a diagnosis of AKI. These cases of mild AKI will have been included in the control group.
Relatively small number of patients with previously recovered AKI
31% of recovered AKI was of unknown cause
Despite a disparity in the racial profile between groups, there was no subgroup or matched control approach to avoid the potentially confounding effects of race.
Discussion
Overall, a previous episode of AKI even when followed by clinical recovery of renal function acts as a risk factor for adverse maternal and fetal outcomes in pregnancy, independently of other risk factors.
It is possible that the increased risk of preeclampsia observed here after recovered AKI might explain global variations in the incidence of preeclampsia. Both preeclampsia and early life episodes of AKI are more common in low income countries.
The pathophysiological mechanisms behind the increased risk observed here isn’t clear. The authors speculate that the underlying process might converge on endothelial injury. Perhaps there is a shared risk factor for both AKI and pre-eclampsia which might explain this association.
This study raises interesting questions concerning risk stratification in pregnancy. Based on these results, it appears that women with a history of any renal injury should be counselled carefully about the risk of adverse pregnancy outcomes.